What you need to know?
- Your spinal cord injury (SCI) might limit your ability to control your urine. You might not be able to stop urine from flowing, or you might not be able to release it.
- Uncontrolled urination or inability to empty your bladder can have a negative effect on your quality of life and cause bladder and kidney infections and other problems.
- Appropriate bladder management can help keep your bladder and kidneys healthy.
- Each type of bladder management option has pros and cons.
- Your doctor can help you choose the bladder management option that best meets your needs and lifestyle, and keeps your bladder and kidneys healthy.
Understanding your body
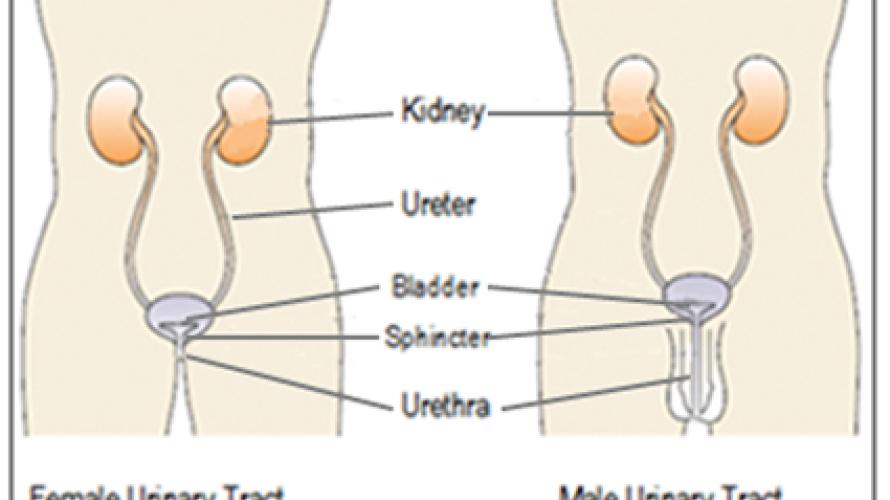
- The kidneys remove waste from your body through your blood stream. This waste becomes urine.
- The urine passes down the ureters (pronounced YOU-ret-erz) into the bladder. The sphincter (pronounced SFINK-ter) muscle at the end of the bladder acts like a valve that you can tighten to keep urine from leaving your body. (When you urinate, your sphincter normally relaxes and your bladder squeezes to push the urine out of your bladder).
- Urine passes from the bladder through the urethra (pronounced yur-EETH-rah) out of your body. In women, the urethra is right above the vagina. In men, the urethra is in the penis. The inability to control the release of urine is called urinary incontinence (pronounced in-KAHN-ten-ans). The inability to release urine from your bladder when it is full is called urinary retention.
What does my spinal cord have to do with my bladder?
- Your brain sends and receives signals through your spinal cord. At the lowest part of your spinal cord (see MSKTC factsheet entitled Understanding SCI Part 1) is an area called the sacral micturition (pronounced SAY-krul mich-ter-ishun) center that has nerves attached to it that go to and from the bladder. These nerves help to signal the brain when the bladder needs to be emptied. They also control the sphincter.
- For example, if you need to hold your urine until a convenient time to empty your bladder, your brain will signal the bladder not to squeeze and the sphincter to tighten so that you can wait. When it is time to release your urine, signals from your brain will then send signals down your spinal cord to squeeze the bladder and relax the sphincter. If an SCI has damaged the spinal cord, the signals from the brain to the bladder do not work correctly and you might not be able to control your urine. You might not be able to stop urine from flowing (urinary incontinence), or you might not be able to release it (urinary retention).
What bladder problems can an SCI cause?
An SCI can cause two types of bladder problems. One set of problems occurs immediately after injury, and the other may begin later on after your injury (long term) when you are out of spinal shock (see below)
Immediately after SCI:
- You might experience spinal shock, when signals from the brain can’t get to any or most parts of the body below the spinal cord injury.
- Spinal shock in general usually lasts for up to a few days, but for the bladder it can last several months or longer.
- Your bladder does not squeeze when you are in the period of spinal shock.
After your bladder is out of spinal shock:
- Signals to and from your brain may still be blocked by the SCI.
- Your sacral micturition center is an area of the spinal cord at the base of the spine. This is the area of the spinal cord that controls your bladder and sphincter.
- After spinal shock, your sacral micturition center it might start sending signals on its own to tell the bladder to squeeze. In addition, signals that would normally come down from your brain to keep your sacral micturition center from sending signals to make your bladder squeeze are blocked by your SCI. Therefore your bladder begins to squeeze and possibly cause you to also urinate without control (urinary incontinence). This is known as a “neurogenic overactive bladder.”
- Your sphincter might tighten or relax on its own, starting and stopping your urine stream without your control.
- Your bladder might try to squeeze but the sphincter might tighten at the same time, making you unable to urinate and causing a high-pressure buildup in the bladder. This is known as detrusor (bladder) sphincter dyssynergia (pronounced dis-IN-ergh-IAH). This can stretch your bladder beyond what is healthy and can cause bladder infections.
- High pressures in your bladder can also prevent urine from draining from your kidneys to your bladder and can cause kidney infections, kidney stones, and even kidney damage.
- Another problem that can occur in those with SCI at T6 and above is autonomic dysreflexia. This can happen when something causes pain or discomfort to your body even though you may not feel it. The two most common causes are bladder distention (and bladder contractions) and constipation. Autonomic dysreflexia causes a sudden severe elevation in blood pressure which has the potential of being dangerous. Autonomic dysreflexia may or may not (silent autonomic dysreflexia) cause other symptoms such as headache, flushing, and/or goose bumps. It will not get better until the cause of the autonomic dysreflexia is taken care of, such as emptying the bladder. (See the reference below for more details on acute autonomic dysreflexia.)
- Over time there are also risks of having other problems such as bladder or kidney infections and a slight risk of developing bladder cancer, bladder or kidney stones, or kidney damage.
Does the level of injury on my spine affect what problems I experience?
- Yes, however everyone’s bladder and sphincter act a little differently because the amount of nerve injury is a little different for each person even if you have the same level of injury as someone else.
- Keeping that in mind, the major areas to consider are:
- At or below the sacral micturition center
- Above the sacral micturition center
At or Below the Sacral Micturition Center:
- If the SCI damaged the spinal cord at or near the base of your spine, the sacral micturition center might be damaged.
- When this center is damaged, signals can’t be sent to the bladder to tell the bladder to squeeze (neurogenic underactive bladder).
- It the damage is below your sacral micturition center then even though signals are sent towards the bladder, the nerves to the bladder are damaged so the signals do not reach the bladder and your bladder will not squeeze.
- Your bladder will then become very full (over distended).
- If you have a weak urinary sphincter, urine will probably overflow from your bladder without your control (urinary incontinence).
- If you have a strong urinary sphincter, urine may not be able to be released leading to a possible increase in bladder pressure and possible back-up of urine in your kidneys.
Above the Sacral Micturition Center:
- The sacral micturition center sends signals to your bladder causing it to squeeze. Your spinal cord injury also blocks signals coming down from the brain which are telling the bladder when and when not to squeeze, causing you to have an overactive bladder. (See above section.)
- Signals also don’t usually get to your urinary sphincter to tell it to relax when your bladder is squeezing (detrusor sphincter dyssynergia). (See above section.)
- If your injury is at T6 or above you may get autonomic dysreflexia from your overactive bladder and detrusor sphincter dyssynergia.
- Your bladder will then become very full (over distended).
How can I know if my bladder and sphincter are working correctly?
Doctors can do a urodynamics (pronounced yur-oh-di-NAM-iks) test to see how well your bladder and sphincter are working:
- A catheter (a small tube) goes up through your urethra into the bladder.
- Your bladder is slowly filled with fluid.
- Doctors then measure how your bladder and sphincter respond to the fluid in the bladder.
- The test can help inform which bladder management option is best for you.
What is bladder management?
Bladder management is an ongoing set of treatments and practices that help keep your bladder and kidneys healthy and free from infection and other problems.
- Bladder management cannot fix or solve the problems caused by your SCI, but it can help you manage them to improve your health and quality of life. With appropriate management you can prevent incontinence and damage to the kidneys.
- You can work with your doctor to choose which bladder management option fits into your lifestyle and maintains bladder and kidney health.
What are some types of bladder management?
There are many types bladder management following SCI, each with various advantages and disadvantages. Several of the more common types of bladder management are listed below. It is important to speak with your health care provider to determine which option is best for you.
If you continue to have significant problems affecting your kidneys or bladder or your lifestyle despite non-surgical bladder management options, your doctor might in rare cases suggest a surgical option such as a urinary diversion. For more information on surgical management, see MSKTC factsheet entitled Surgical Alternatives for Bladder Management Following SCI. This factsheet will focus on some of the more common non-surgical options of bladder management.
Intermittent Catheterization (pronounced kath-et-er-iz-AY-shun)
This option is used for draining your bladder without keeping a catheter in your bladder all the time.
- You (or someone else) insert a catheter into your bladder to keep your bladder from getting too full.
- To do this, pass the catheter up your urethra into the bladder. The urine drains out the other end.
- When done, remove the catheter and return to normal activities.
- Do this as often as needed (usually 4-6 times per day). The goal is to keep your catheterization volumes less than 500 ml. (about 17 fl oz) so you may have to catheterize more or less often depending on how much you drink.
- You will often need medication or injections (such as Botox) to keep your bladder quiet in order to prevent leaking and high pressures in your bladder.
- This option might NOT be for you if:
- You are unable to catheterize yourself (or don’t have someone to help you).
- Your bladder is very small (so you would have to catheterize your bladder very frequently).
- Your bladder is overactive (even with treatment; so you may have high bladder pressures or incontinence).
- Your sphincter is overactive (will not relax easily; so the catheter will not pass easily into your bladder).
- Your sphincter is underactive (will not tighten; so you will have frequent urinary incontinence).
- You have a false passage in your urethra (so the catheter may get caught in the false passage).
- You drink a lot of fluid (more than 2 -21/2 quarts or 2 liters) every day so you would need to catheterize very frequently).
- You have a lot of pain when inserting or removing the catheter.
- You can use different types of catheters. Your doctor can help you decide which type of catheter is best for you. For example, the catheter might:
- Have a slight curve at the tip. This is known as a Coudé (pronounced ku-DAY) catheter.
- Have a bag attached at the end to catch the urine.
- Be covered with lubricant to help it slide through your urethra.
Advantages
- Intermittent catheterization simulates normal bladder filling which helps to maintain your normal bladder size.
- You will not wear an internal or external catheter and leg bag all the time.
Disadvantages
- You need to keep track of your fluid intake so that your bladder doesn’t fill up too soon and get overstretched, especially while you are sleeping.
- You need to partially undress each time you use a catheter.
- You might find removing and inserting a catheter uncomfortable.
- If you are a woman, you might have trouble finding and passing your catheter into your urethra. You might cause some irritation or bleeding when passing a catheter into your bladder, especially if you are a man and have a very spastic urinary sphincter that tightens when you try to remove the catheter.
- You may need to take medication to keep your bladder from being overactive and causing urinary leakage.
Indwelling Catheterization
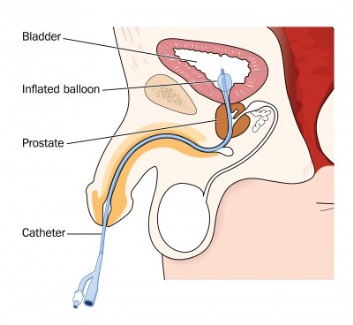
This option is used for ongoing protection from urinary retention or urinary incontinence. Indwelling catheterization uses a catheter and a urine collection bag that stays in place all the time. The catheter has a balloon at the tip of the catheter which sits in your bladder. Once the catheter is in your bladder, the balloon can be inflated to keep the catheter from falling out or deflating when it’s time to change the catheter.
There are two types of indwelling catheters: urethral catheters and suprapubic (pronounced soo-prah-PEW Bik) catheters. Most urethral catheters that are kept in place by filling up a balloon. People might call your indwelling catheter a Foley catheter.
Type 1: Urethral Catheters
A urethral catheter is inserted through your urethra, by yourself, by a physician, nurse or a trained family member using a similar technique as intermittent catheterization. However, instead of removing the catheter when your bladder is empty, the indwelling catheter stays in your bladder and is held in place in your bladder by a small balloon at the end. A small tube connects the other end of the catheter into a collection bag. It is not a good idea to plug your catheter, especially if you do not have good sensation in your bladder. If your bladder fills up and gets over distended, it can cause serious problems such as a bladder or kidney infections or autonomic dysreflexia (if your injury is at T6 and above).
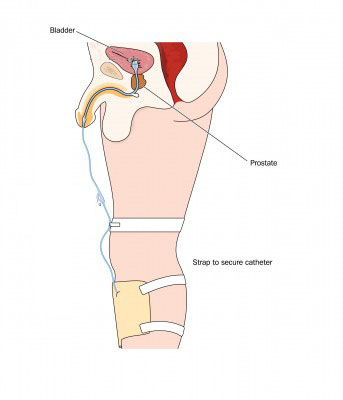
There are several types of collection bags:
- Smaller bags can be strapped to your leg so that you can move freely.
- Some larger bags don’t have to be drained as often and are used when you are sleeping (called night bags).
- A modified bag can be strapped around your waist (called a belly bag) instead of your leg.
A collection bag must be emptied frequently:
- A collection bag must be emptied several times a day to keep it from getting too full. It is best to try to empty the bag when it gets about one half full./li>
- If the bag gets too full, pressure may build up in the bag and keep the urine from flowing down the tube. Instead, the urine will back up. This could cause your bladder to become over stretched and cause problems such as bleeding, bladder infection, or autonomic dysreflexia.
A urethral catheter stays in place all the time. About once a month, the catheter is removed and a new one is put in place. This may be done sooner if the catheter gets blocked from bladder stones or if there are other problems with the catheter’s drainage.
Advantages
- You do not need to worry about inserting and removing the catheter into your bladder several times a day.
- You do not need to limit the amount of liquid you drink.
- You do not need to undress to use the catheter.
Disadvantages
- About 3 out of 10 people who use a urethral catheter get bladder stones, which are small hardened pieces that collect and can block your catheter and cause your bladder to get overstretched. This can cause leaking around the catheter, pain, a urinary tract infection, hematuria (blood in the urine), or autonomic dysreflexia.
- You might have discomfort or pain from the catheter, especially when inserting or replacing it.
- You might be uncomfortable wearing a urine collection bag and worry about it leaking.
- It can be difficult to keep the area around the catheter clean, especially for women.
- A constantly empty bladder can reduce the size of your bladder, making it less able to hold more urine.
- You may need to take medication to keep your bladder from being overactive and causing urinary leakage.
- There can be sexuality issues due to having a catheter in the urethra.
- There may be a slight increase in bladder infections with urethral catheters but not suprapubic catheters compared to other types of management.
Type 2: Indwelling Suprapubic Catheter
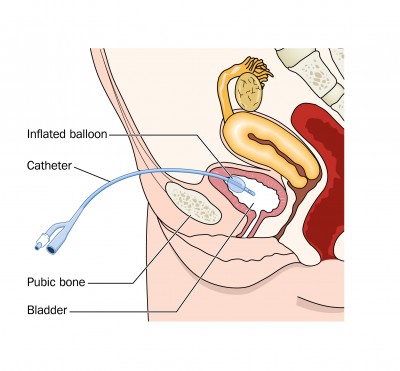
In order to insert an indwelling suprapubic catheter, a doctor first needs to make a small incision below the beltline This is done under an anesthetic. He or she then inserts the catheter through the incision into the bladder. Urine drains out from the catheter and is then stored in a collection bag on the outside of your body. The collection bag is drained as needed, to keep the bag from getting overfilled. The catheter is changed on a monthly basis just like a urethral catheter.
After the catheter has been put in by a doctor, the incision heals and there is a small hole so that the old catheter can be removed and a new catheter can be inserted. It is important to measure the distance that the catheter is in your bladder by marking the catheter at the skin level before removing it and then putting the new catheter in the same distance in. As long as a catheter is in the hole, it stays open. Once the catheter is removed the hole will close in 1-3 days. There are no restrictions with bathing or showering with a suprapubic tube. One study showed that in women, there were fewer bladder infections with a suprapubic tube than any other type of bladder management.
Advantages
- Has all the advantages of a urethral catheter, and a suprapubic catheter also keeps you from feeling pain or discomfort from inserting and removing the catheter from your urethra.
- This catheter is easier to change than a urethral catheter. You do not need to lie down or undress to change the catheter.
- It is easy to keep the area around the catheter clean, and you are less likely to get an infection than with a urethral Foley catheter.
- It is preferable to a urethral catheter for sexuality reasons because the catheter is not in the urethra. If the suprapubic catheter becomes blocked or can't be removed, the urethra can sometimes act as a "pop off valve" releasing some of the urine, or the urethra can be used to pass a temporary urethral catheter.
Disadvantages
- Like urethral catheters, there is an increased risk for developing bladder stones and a smaller bladder.
- You may need to take medication to keep your bladder from being overactive and causing urinary leakage.
- Same day surgery is needed to create the opening for the catheter.
Reflex Voiding
This option primarily is used by men with bladders that fill and squeeze on their own because a convenient way to capture urine is needed.
- This method usually uses an external condom catheter. These catheters fit like a condom around the penis and connect to a tube and collection bag. (There is no effective external collecting device for women.)
- This method requires a relaxed sphincter, and you might need help relaxing it. Methods of relaxing your sphincter include suprapubic bladder tapping (where you lightly tap the area over your bladder), medication, injections, and surgery.
- A man or a woman who uses a reflex voiding option might decide to have their bladder drain directly into a protective undergarment. Undergarments must be changed frequently to avoid the urine causing a skin rash.
Advantages
- You do not need to limit your liquids.
- You do not need to undress to empty your bladder.
Disadvantages
- Men need to wear an external condom catheter, and a leg bag or a protective undergarment to collect urine.
- Women must use a protective undergarment.
- Protective undergarments must be changed frequently.
- The skin around the penis might get irritated from the condom catheter being too tight.
- The external condom might twist or kink and fall off during voiding.
- If you have a “retractile” penis that pulls back into the abdomen, especially when you sit up, the condom catheter might not stay on.
- Additional treatment or medication might be needed to relax your sphincter, and these treatments could cause side effects.
Valsalva and Credé Voiding
This option is for people who have difficulty getting their bladder to squeeze. Credé (pronounced kre-DAY) is a method where you push inwards with a closed fist over your bladder to empty it. Valsalva (pronounced vahl-SAL-vah) is a method where you tighten your abdominal muscles and bear down to force urine from your bladder.
- The amount of bladder emptying depends on how much force you use to push urine from the bladder and how much your sphincter relaxes.
- While not recommended, people sometimes use crede or valsalva voiding in addition to their other type of bladder management. For example bearing down when they catheterize themselves to try to make their bladder empty a little quicker by forcing the urine flow through the catheter quicker or bearing down and forcing a little urine out of their bladder so they do not catheterize themselves as often.
Advantages
- You do not need to use a catheter of any kind.
Disadvantages
- The pushing or straining to empty your bladder can cause problems over time (such as hemorrhoids, hernias, and other medical problems).
- To catch the urine, you will need to undress and transfer onto a toilet, use a bed pan, or wear protective undergarments.
- It often takes a lot of effort and time to bear down in an attempt to empty your bladder.
- You may not be able to empty your bladder completely leading to complications such as UTI’s and bladder stones.
Summary
- Following an SCI, maintaining healthy kidneys and a healthy bladder are important. There are many bladder management options.
- Your doctor can help you find the best option for your needs and lifestyle.
- Your doctor can also help you decide when an option is working well, or if a new option needs to be considered.
Reference
Consortium for Spinal Cord Medicine (2002). Acute management of autonomic dysreflexia: individuals with spinal cord injury presenting to health-care facilities. J Spinal Cord Med. 25, Suppl 1:S67-88.
Authorship
Bladder Management Options Following Spinal Cord Injury was developed by Todd A. Linsenmeyer, M.D., and Steven Kirshblum, M.D., in collaboration with the Model Systems Knowledge Translation Center.
Source
Our health information content is based on research evidence and/or professional consensus and has been reviewed and approved by an editorial team of experts from the Spinal Cord Injury Model Systems.
Disclaimer
This information is not meant to replace the advice of a medical professional. You should consult your health care provider regarding specific medical concerns or treatment. The contents of this fact sheet were developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant number 90DP0012-01-00). The contents of this fact sheet do not necessarily represent the policy of Department of Health and Human Services, and you should not assume endorsement by the Federal Government.
Copyright © 2015
Model Systems Knowledge Translation Center (MSKTC). May be reproduced and distributed freely with appropriate attribution. Prior permission must be obtained for inclusion in fee-based materials.